Gastroparesis Diet: Foods To Avoid, Foods To Eat, And Tips
A low-fiber and low-fat diet plan to soothe your troubled digestive system.

Image: Shutterstock
Gastroparesis is a rare condition characterized by improper digestion and its painful symptoms can severely impact everyday life. A specialized gastroparesis diet promotes the consumption of soft low-fiber and low-fat foods for easier digestion.
The unusual nature of the condition and its similarities with other gastrointestinal problems can make diagnosis difficult. There is no official diet plan or a specifically safe medication to treat it. Hence, the gastroparesis diet needs constant regulation to keep the symptoms in check. That said, proper adherence to the guidelines, nutrition awareness, and diet therapy can make this condition manageable. Keep reading to learn more about the gastroparesis diet, its structure, meal plans, and more.
 At A Glance: Gastroparesis Diet
At A Glance: Gastroparesis Diet- Principle: Intake of detoxifying juices and cooked, easy-to-digest food to improve digestion
- Purpose: To alleviate the symptoms of gastroparesis
- Who It Is For: People with gastroparesis
- Duration: Short-term
- Who Should Avoid: Healthy individuals
- Cons: May lead to nutrient deficiencies and calorie deficits.
In This Article
What Is Gastroparesis?

Gastroparesis is a clinical condition where food remains in the stomach for prolonged periods due to weakened stomach muscles and delays the emptying of the gastric passage. This chronic condition is also called gastric stasis and impacts digestion. Its common symptoms include abdominal pain, vomiting, nausea, early satietyi A condition where you cannot eat a full meal as you feel full after eating only a small amount of food. , and bloating (1).
Mary Sabat, Registered Dietitian Nutritionist, says, “Gastroparesis can be caused by various factors, including diabetes, neurological conditions, post-surgical complications, viral infections, and certain medications. It can lead to malnutrition and make it challenging for individuals to maintain a healthy weight and lifestyle.”
 Fun Fact
Fun FactGastroparesis is not common. Its diagnosis can be tricky as its symptoms overlap with other digestive disorders like epigastric pain syndromei A set of symptoms associated specifically with upper abdominal pain, most commonly caused by indigestion. (EPS) and irritable bowel syndromei A commonly occurring gastrointestinal disorder characterized by excessive cramping, flatulence, bloating, diarrhea, and constipation. (IBS) (2). It is more likely to occur in people with long-term medical conditions like diabetes (3). It can also develop in people with upper gastrointestinal tract tumors (4).
According to a study published in the American Gastroenterology Association Journal, 268 in every 1,00,000 US adults have gastroparesis (5). Most people with gastroparesis were also found to have other chronic diseases like diabetes and peripheral vascular disease.
Prescribed treatments for gastroparesis include diet changes and medication. While medication options are limited, some medicines prescribed to help with delayed stomach emptying can have serious side effects. However, people with gastroparesis may be willing to try novel medications as the symptoms can be painful and impact everyday life.
The risk of side effects from medications makes dietary modifications the primary treatment measure for gastroparesis. In the following sections, we shall explore the scope and impact of the gastroparesis diet.
Key Takeaways
- The gastroparesis diet is designed to reduce gastroparesis symptoms and provide adequate nutrition for long-term management.
- The diet begins with a 3-day liquid-only stage, progresses to the intake of soft low-fiber and low-fat foods, and finally ends with the intake of minimal fiber and fat.
- High-fiber cruciferous vegetables, high-fat dairy, fried foods, and tough meats are excluded from this diet.
- Go for diet therapy or nutritional counseling for an accurate profiling of your symptoms and nutrient requirements.
What Is The Gastroparesis Diet?
The gastroparesis diet comprises specialized dietary modifications, guidelines, and medical advice to alleviate the symptoms of gastroparesis. However, there is no universal gastroparesis diet and most medical professionals recommend working with a certified dietitian for a proper analysis and treatment plan.
Some studies have shown that fatty, spicy, or acidic food can aggravate the symptoms of gastroparesis while gluten-free items, tea, and white rice can help alleviate the symptoms (6). The general gastroparesis diet focuses on consuming easy-to-digest foods to avoid straining your digestive system and minimize symptoms.
Furthermore, symptoms like early satiety and nausea can leave your body dehydrated and malnourished. So, this diet also focuses on nutrient-dense foods to ensure good health. That said, there is no one diet format that suits everyone with this condition. Hence, these dietary measures require constant monitoring. Any new changes observed in the digestive system are answered with diet modifications to suit them.
This complex diet works in multiple stages to help your stomach muscles recover and slowly restore their proper digestive functions.
The following section explains the basic structure of the gastroparesis diet and how it helps manage the condition. Check it out.
How Does The Gastroparesis Diet Work?

The first step is to drop spicy, acidic, fatty, and roughage-rich foods to avoid triggering the symptoms. You can consume foods with mild sweet, salty, and bitter flavors (6).
The diet works in three phases. The first phase is quite similar to the bland diet in some aspects. It involves total restriction of multiple food groups and intake of only juices and bland or well-cooked foods for easy digestion. The following two phases allow a gradual reintroduction of solid foods. This is to identify foods that are easy on your digestive system.
Each stage has guidelines to be followed for a few days to allow your stomach to detox and gradually build its tolerance. Depending on the severity of your condition, your dietitian may adjust your solid food diet accordingly for long-term management of your symptoms.
 Quick Tip
Quick TipIn the following section, we shall explore the modification rules and guidelines of this complex multiphase diet.
Gastroparesis Diet Modifications And Guidelines
The gastroparesis diet is a three-phase dietary approach that focuses on healing, supporting, and maintaining your digestive system. Here is how the three phases are structured:
Phase I – Detoxing With Liquids: Consume only liquids for 1-3 days to lower the stress on your stomach. Plain water, tea, low-fat soups, and thin juices are recommended. You may also eat plain white crackers if you feel hungry.
This phase may include:
- Clear Liquid Phase: It includes clear liquids like water, broth, clear fruit juices (without pulp), and clear sodas. These liquids are easily digested and do not place much strain on the stomach. This is the initial phase when the gastroparesis symptoms are severe.
- Full Liquids Phase:In this phase, more variety is introduced, including thicker liquids such as milk, yogurt, and fruit juices (without pulp), soups, and protein shakes.
- Pureed Foods Phase:If the patient can tolerate, pureed or mashed foods are added to their diet.
Phase II – Eating Soft Foods:
Consume soft, easily chewable, and easy-to-digest foods, like well-cooked white pasta, scrambled eggs, oatmeal, cooked cereal, and white bread. You may also consume canned low-fiber vegetables and fruits or have them after skinning, cooking, and pureeing them. Avoid high-fiber foods such as whole grains, raw vegetables, and fruits, as they can be challenging to digest.
Phase III – Building Tolerance: Add fibers to your diet gradually and reintroduce solid foods. Monitor the symptoms and how your body reacts and make adjustments to the diet as needed. Revert to phase 2 if your symptoms flare up.
While you are still observing your body’s reactions to different foods, following some general rules and precautions can help.
Gastroparesis Dietary Guidelines
Adhere to the following guidelines for quick relief:
- Phase I is a liquid-only diet, which means your body is not going to receive adequate nutrition. Adhere only until your symptoms improve (this may take 1-3 days). Avoid extending this period as it may lead to nutrient deficiencies.
- Avoid high-fiber, high-fat, and fried foods throughout the stages as they take longer to digest (7).
- In Phase 3, you may cook your high-fiber foods until they are tender to digest. However, avoid cruciferous vegetables like cauliflower, cabbage, broccoli, etc., as they may be too hard to break down.
- Since your stomach has trouble moving food to the intestines, consume frequent small meals every 2-3 hours to avoid any strain.
- Many people on the gastroparesis diet may experience nutrient deficiencies despite self-regulated diet plans. Consult a nutritionist or dietitian for diet therapy. A study found that people with diabetes and gastroparesis were able to improve their daily calorie and nutrition intake through diet therapy (8).
- Chew your food well before swallowing to further break down your food down for easy digestion.
 Quick Tip
Quick TipWhile diet modification and therapy may be straightforward for people only dealing with gastroparesis, it may not be the same for those with additional illnesses such as diabetes. The following section explains more about such complex medical conditions.
Diabetes And Gastroparesis Diet
People with diabetes need to exercise caution with this diet as the dietary needs for diabetes and gastroparesis may clash and make their management challenging. The simultaneous presence of both conditions may also increase the risk of cardiovascular diseases, retinopathyi A complication characterized by damaged blood vessels in the retina, commonly caused due to uncontrollable diabetes. , and hypertensioni A condition where the force of the blood is high against the artery walls, increasing the risk of stroke and heart disease. (9). Consult your doctor before going on this diet.
Now that you know the key details and guidelines of the gastroparesis diet, explore the next section to understand the different food items that you can consume.
Foods To Eat On The Gastroparesis Diet

Low-fiber and low-fat foods are generally allowed on the gastroparesis diet. Here are a few foods that can keep your symptoms in check:
Low-Fiber Foods For The Gastroparesis Diet
- Well-Cooked Vegetables: Green beans, carrots, zucchini, spinach, and potatoes that are skinned and cooked until softened
- Lean Proteins: Tofu, eggs, lean, skinless, and soft meats from chicken, turkey, fresh seafood like white fish and shrimp, and canned tuna
- Fruits: Fully ripened, cooked, pureed, canned, or non-pulpy juice versions of fruits without the skins and seeds
- Grain Foods: White bread, white rice, low-fiber or refined flour products and cereals, puffed rice, plain bagels, English muffins, and low-fat plain crackers. Ensure these items do not contain gluten as it is not easily digested(10).
Low-Fat Foods For The Gastroparesis Diet
- Soups: Fat-free brothy soups
- Nut Butters: Smooth (avoid the chunky variety) peanut and almond butters
- Dairy Products: Low-fat or fat-free milk, yogurt, and soft cheese
- Dessert: Gelatin-based desserts, low-fat pudding and custard, and ice cream (in moderation)
- Beverages: Water and unspiced herbal teas
Check out the nutritional profile of these foods to plan well-balanced meals. Also, apart from adding these foods to your diet, you also need to avoid certain foods to ensure healthy recovery. Learn more in the next section.
Foods To Avoid On The Gastroparesis Diet
Refrain from eating high-fiber and high-fat foods as they take longer to break down and may further aggravate the symptoms. Avoid the following foods to ensure a healed digestive system:
High-Fiber Foods To Avoid On The Gastroparesis Diet
- Vegetables: Cruciferous vegetables like cauliflower, broccoli, cabbage, lettuce, and dried beans, and raw vegetables or those with hard skins like gourds and bell peppers
- Proteins: Legumes, tough-cuts of meats, processed, roasted, and fried meat products
- Fruits: Citrus fruits, as their acidic content may possibly aggravate symptoms (6)
- Grain Foods: Whole grain foods, brown rice, and pizza
High-Fat Foods To Avoid On The Gastroparesis Diet
- Soups: Cream-based, thick soups
- Nuts: Solid nuts and seeds
- Dairy: Full-fat whole milk and cream
- Sugary Foods: Desserts and baked goods with high amounts of sugar
- Drinks: Coffee, caffeinated, carbonated, and alcoholic drinks and acidic juices from citrus fruits and tomatoes
Additionally, avoid spicy foods that may aggravate your stomach lining. Remember to eat frequent, small meals.
 Quick Tip
Quick TipThe following section illustrates sample menus and meal plans to help you create customized diet strategies. Keep reading to know more.
Gastroparesis Diet Meal Plan
As we have discussed above, the gastroparesis diet plan functions in phases. Let us look at phase-wise sample diet plans.
Phase I Gastroparesis Diet Plan (1-3 Days)
Since phase 1 is a liquid-only diet, you may only consume the following liquids at regular intervals whenever you feel hungry.
- Water
- Plain herbal teas
- Thin, non-pulpy fruit juices (avoid citrus or acidic fruits)
- Fat-free clear soups or broth
You may eat gluten-free plain white crackers if you feel hungry. Avoid anything else.
Phase II Gastroparesis Diet Plan (3 Days)
You can incorporate certain soft foods and meal replacement drinks into the phase 2 diet. Here is a sample 3-day diet plan.
| Day | Early Morning Drink | Breakfast | Mid-Morning Snack | Lunch | Evening Snack | Dinner |
|---|---|---|---|---|---|---|
| Day 1 | 1 cup of green tea | 1 slice of white bread with 1-2 scrambled eggs and ½ cup of canned apricots in water | ½ glass of meal replacement shake | ½ cup of chicken noodle soup, ½ cup of no-fat yogurt, ½ cup of canned peas in water | ½ cup of no-fat cottage cheese with ½ cup of fruit puree | 85 grams of smoked fish with ½ cup of boiled and mashed root vegetables |
| Day 2 | 1 cup of peppermint tea | 1 glass of fruit juice, 4-6 rice crackers, and ½ banana | ½ glass of meal replacement shake | ½ cup of turkey and cooked veggies soup and ¾ cup no-fat yogurt mixed with ¼ cup unsweetened applesauce | 1 slice of white bread with 1 teaspoon of light mayo | 2 scrambled eggs, ½ cup of boiled beets, ½ cup of canned peaches in water, and ½ cup of mashed potatoes |
| Day 3 | 1 cup of chamomile tea | ¼ cup of fat-free Greek yogurt, 1 glass of smoothie, and 4-6 saltine crackers | ½ glass of meal replacement shake | 1-2 slice of white bread spread with 2 tablespoons of smooth peanut butter and ½ cup of canned peaches in water | ½ cup of no-fat unflavored yogurt with 1 teaspoon of honey | 1 cup of elbow noodles with ½ cup of pureed veggies |
Phase III Gastroparesis Diet Plan (3 Days)
Minimal fiber and fat can be introduced in phase 3. However, return to phase 2 immediately if your body does not adapt to these changes. Here is a sample phase 3 meal plan.
| Day | Early Morning Drink | Breakfast | Mid-Morning Snack | Lunch | Evening Snack | Dinner |
|---|---|---|---|---|---|---|
| Day 1 | 1 glass of green juice | 1 glass of smoothie with 2% fat yogurt, 1 fresh skinless peach, and ½ banana | ½ glass of meal replacement shake | ½ cup of canned tuna in water, ½ cup of boiled vegetables with no-fat dressing, and 4-6 saltine crackers with 1 teaspoon of low-fat mayo | ½ cup of 2% fat Greek yogurt with 1 teaspoon of honey | 1 slice of white bread, 2 scrambled eggs, and ¾ cup of vegetable soup |
| Day 2 | 1 cup of herbal tea | 1-2 slices of white bread with 2 tablespoons of smooth peanut butter and ½ glass of fresh fruit juice | ½ cup of 2% fat cottage cheese with ½ cup of skinned and diced apple | ¾ cup of clear veggie broth, ½ cup of ramen, 1 boiled egg, ½ cup of diced mangoes | ½ glass of meal replacement shake | 85 grams of smoked fish, ½ cup of boiled squash, ½ cup of zucchini, mushrooms, and spinach |
| Day 3 | 1 glass of non-pulpy, non-acidic fruit juice | 1 slice of white bread, 2 scrambled eggs, 1 slice of low-fat cheddar | ½ glass of meal replacement shake | ½ cup of white rice, ½ cup of lean, skinless chicken, ½ cup of pureed veggies | ½ cup of 2% fat Greek yogurt with ½ cup of diced melon | 85 grams of boiled chicken, ½ cup of mashed potatoes, and ½ cup of baked eggplant |
While low quantities of fiber and fat are allowed in phase 3, note that full-fat and fried foods are still restricted. Avoid them to allow your digestive system to heal properly.
You will have an idea about the kind of foods that suit you by the end of the three phases. Add more food items from the allowed list of foods to establish a personalized meal plan for long-term gastroparesis management. To help you with the same, we have included a few easy and yummy recipes in the next section.
Healthy Recipes For Gastroparesis Diet
Since this diet recommends consuming multiple small meals throughout the day, recipes for gastroparesis management are fairly simple. Let us check out a few delicious and easy options.
1. Pasta With Spinach And Basil Pesto

Ingredients
- ½ cup of uncooked pasta of choice
- 1 tablespoon of olive oil
- 2-3 cups of water
- 2 cups of fresh basil leaves
- 1 cup of fresh spinach leaves
- ⅓ cup of low-fat chicken broth
- 3 cloves of garlic
- 1 teaspoon of grated lemon zest
- Salt and pepper to taste
Preparation Time:
15-20 minutes
How To Prepare
- Boil water in a saucepan.
- Put pasta, olive oil, and 1 teaspoon of salt into the boiling water and let it cook for 7-10 minutes. Once the pasta is cooked, strain it and let it cool.
- Microwave the chicken stock and garlic together for 5 minutes. Once heated, take it out and let it cool.
- Roughly chop basil and spinach and add to a food processor.
- Add the garlic broth, lemon zest, and salt and pepper into the processor and blend for a smooth pesto sauce.
- Toss the pasta in the pesto and serve with a side of shredded chicken.
2. Creamy Carrot Soup

Ingredients
- 2 cups of carrot cubes
- 1 large potato, peeled and diced
- ½ cup of finely chopped onions
- 1 teaspoon of minced garlic
- 3 cups of low-fat vegetable broth
- Salt and pepper to taste
- 2-3 tablespoons of sour cream for garnish (optional)
Preparation Time:
30-40 minutes
How To Prepare
- Heat the olive oil over medium heat in a medium-sized soup pot or saucepan.
- Saute the onion and garlic for 3-5 minutes till the onions turn translucent.
- Add the diced potatoes and carrots into the pot and saute for another 5 minutes.
- Pour the vegetable broth into the pot and bring the mixture to a boil.
- Turn to low heat and cover the pot with a lid. Let the soup simmer for 20-25 minutes until the carrots and potatoes are tender enough to be easily smashed.
- Allow the soup to cool slightly and blend until it has a creamy consistency.
- Add salt and pepper and other seasonings if you prefer.
- Pour the soup into a bowl and garnish with sour cream and parsley.
3. Mexican Shredded Chicken

Ingredients
- 85 grams of lean chicken breasts, skinned
- ¼ cup of low-fat vegetable or chicken broth
- 1 teaspoon of ground cumin
- 1 teaspoon of chili powder
- 2 tablespoons of lime juice
- ¼ cup of diced, fresh cilantro
- Salt to taste
Preparation Time:
30-40 minutes
How To Prepare
- Boil the chicken breasts in a large pot of boiling water for about 15 minutes.
- Remove the chicken from the water and shred it finely using a fork.
- Pour the broth into a saucepan over medium heat and add the shredded chicken, cumin, chili powder, lime juice, and salt. Let it simmer for 5-10 minutes until the broth thickens into a sauce.
- Serve the chicken over a plate of rice and garnish with fresh cilantro.
Smoothie For Gastroparesis Diet
Quick and wholesome fruit and vegetable smoothies are easy to digest and promote nutrient absorption in people with gastroparesis. Check out this smoothie recipe to add some variety to your meal plan.
1. Simple Green Smoothie

Ingredients
- ¼ cup of frozen zucchini
- 1 handful of baby spinach
- ½ cup of frozen pineapple chunks
- 1 cup of coconut water
- 1 scoop of vanilla protein powder
- Juice from 1 lime
- 1 teaspoon of trace minerals (optional)
Preparation Time:
5 minutes
How To Prepare
- Blend all the ingredients together.
- Serve chilled with plain crackers.
You may replace pineapple, zucchini, and spinach with other fruits in similar proportions for varied flavors.
Snacks For Gastroparesis Diet

The snacking options for gastroparesis are quite simple. Pick foods that require minimal chewing, have bland flavors, and digest easily. Here are a few snacks you may add to your meal plan:
- 3-4 plain rice crackers with ½ cup of unsweetened applesauce
- 2-3 plain rice cakes with 1 tablespoon of cream cheese
- 1 slice of white bread with 1 tablespoon of smooth nut butter of your choice
- ½ cup of low-fat yogurt with ¾ cup of diced bananas, mangoes, or canned fruit
- 1 boiled egg, halved and seasoned with a pinch of salt and pepper
You may experiment with these recipes in phase 3 of the diet. However, in phase 2, you must be mindful of potential stomach irritants and only eat soft foods. Here is a list of soft foods to help you transition from the phase 1 to the phase 2 of the gastroparesis diet.
Soft Foods For Gastroparesis
Focus on soft food items that may help alleviate gastroparesis symptoms. Here is a list of gastroparesis-friendly soft foods:
- Well-cooked, low-fiber skinless vegetables such as zucchini, carrots, and green beans
- Boiled potatoes mashed with 1 teaspoon of butter
- Soft scrambled eggs with minimal salt
- Cooked white rice
- Canned fruit in water
- Smooth clear soups
- Smooth nut butter
- Tofu that can be blended into smoothies or added to meals for protein
- Low-fat cottage cheese or Greek yogurt
- Low-sugar puddings and custards
- White bread, bagels, crackers, and pretzels
- Well-cooked lean meats
These detailed meal plans and recipes should help you navigate your journey in a systematic manner. Additionally, you might find these cooking and meal preparation tips useful. Take a look below.
Gastroparesis Diet Tips
Here are some helpful diet tips to help you ease into the diet and ensure effective meal planning:
- Eat 5-8 small meals throughout the day.
- Begin your meals with high-nutrient foods to ensure more nutrient intake in case you feel full quickly.
- On phases 2 and 3 of the diet, consume solid meals during the day for more nutrition and keep liquids for later in case you feel hungry.
- Always chew your food well to ensure easy digestion.
- Cook or prepare your food in bulk and refrigerate it if you cannot cook multiple times in a day. Consume the refrigerated food within two days.
- Opt for cooking methods that require less time. Boil, grill, roast, or steam your vegetables and meats to lower the fats in your diet.
- Consult a dietitian for multivitamin supplements if you are not able to meet your nutrient requirements.
- Drink lots of water throughout the day to restore your digestive functions.
- Avoid alcohol completely as it can dehydrate you and lower your nutrient levels.
- Avoid skipping meals, as doing so may make you overeat later, thus worsening gastroparesis symptoms.
- Keep track of your food intake to identify food triggers as every person with gastroparesis may have a different tolerance to certain foods.
It might also help to join support groups and interact with other people with the same condition. Since this is an uncommon condition that has a severe impact on the quality of life, trying to manage it alone can be discouraging. Being part of a community that understands your challenges and offers additional insights and information can be extremely beneficial in your gastroparesis journey.
The gastroparesis diet is intended to ease the strain on the digestive system. The multiphase diet proposes a temporary liquid-only dietary plan to detox the system and then slowly reintroduces low-fiber and low-fat foods into the diet. While this diet is among the primarily recommended treatment options for gastroparesis, it needs regular monitoring and modifications. Consult a professional nutritionist to ensure your daily nutrition and calorie requirements are met while on this diet.
Infographic: The 3-Phase Gastroparesis Diet Plan
The gastroparesis dietary modifications and guidelines are beneficial for those experiencing severe gastroparesis symptoms. The diet eases digestion and ensures adequate nutrition. Check out the following infographic to learn more about the three phases of this diet plan and what foods can be consumed through each of them.
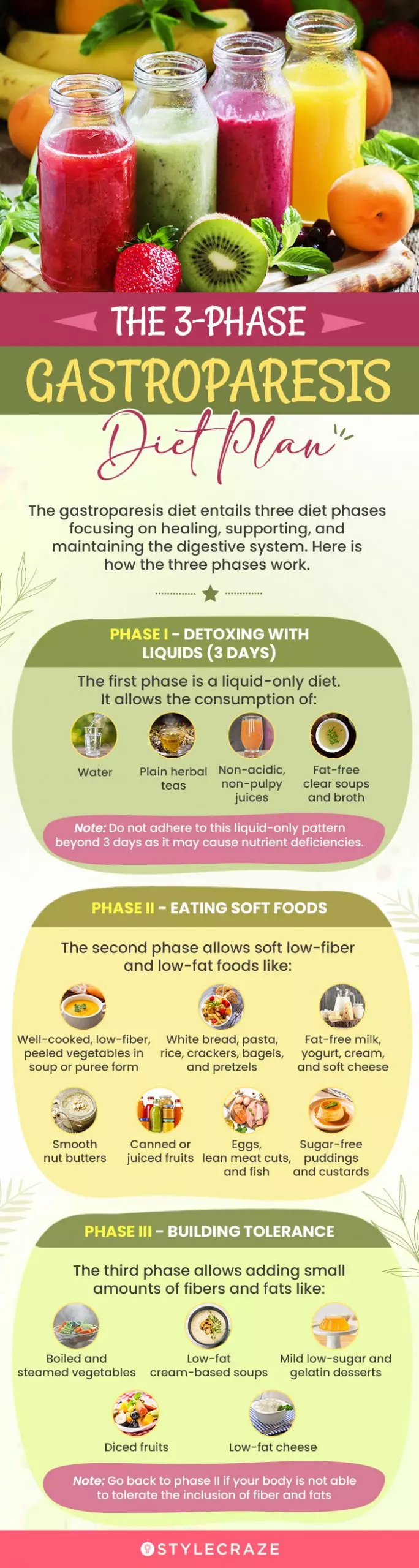
Illustration: StyleCraze Design Team
Frequently Asked Questions
Can you eat popcorn on the gastroparesis diet?
No. Popcorn has a chewy texture and is high in insoluble fiber. It is unsuitable for gastroparesis as it is resistant to digestion (11), (12).
Can you eat oatmeal on the gastroparesis diet?
Yes. Oatmeal is an easy-to-digest soluble dietary fiber (13). Soluble dietary fibers dissolve into gummy gels in water and easily pass through the intestines (12).
What fruits are OK for people with gastroparesis?
All fruits except citrus fruits are ideal for those with gastroparesis. Fruits must be taken in non-pulpy juice forms for easy digestion. Skinless fruits canned in water are also allowed for people with gastroparesis.
Can I live a normal life with gastroparesis?
Unfortunately, gastroparesis may severely impact the quality of life. You have to constantly monitor your diet to keep the symptoms under control. Further, any flare-ups due to negligence may make carrying out daily tasks a challenge.
Is gastroparesis genetic?
No. However, gastroparesis may develop as a complication of hereditary diseases such as diabetes (3).
What is the most common age for gastroparesis?
Research suggests that gastroparesis is commonly diagnosed between 48-65 years of age, and is more than twice as common in females (14).
The gastroparesis diet is highly effective in controlling the symptoms of the illness. But can it be modified to manage your weight? Check out this video where a professional nutrition counselor addresses related questions.
References
Articles on StyleCraze are backed by verified information from peer-reviewed and academic research papers, reputed organizations, research institutions, and medical associations to ensure accuracy and relevance. Read our editorial policy to learn more.
- Gastric Stasis
https://pubmed.ncbi.nlm.nih.gov/29489278//a> - Worldwide prevalence and burden of gastroparesis‐like symptoms as defined by the United European Gastroenterology (UEG) and European Society for Neurogastroenterology and Motility (ESNM) consensus on gastroparesis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9557951/ - Diabetic gastroenteropathy: An underdiagnosed complication
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8192258/ - Malignancy-associated gastroparesis: an important and overlooked cause of chronic nausea and vomiting
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3926490 - Epidemiology, Etiology, and Treatment of Gastroparesis: Real-World Evidence From a Large US National Claims Database
https://www.gastrojournal.org/article/S0016-5085(21)03613-1/fulltext - Foods Provoking and Alleviating Symptoms in Gastroparesis: Patient Experiences
https://link.springer.com/article/10.1007/s10620-015-3651-7 - Diet and Nutrients in Gastrointestinal Chronic Diseases
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7551310/ - Dietary Intake and Nutritional Deficiencies in Patients With Diabetic or Idiopathic Gastroparesis
https://www.gastrojournal.org/article/S0016-5085(11)00600-7/fulltext - Diabetic Gastroparesis: A Review
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428659/ - The Role of Gluten in Gastrointestinal Disorders: A Review
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10096482/ - Analysis of Popcorn (Zea Mays L. var. Everta) for Antioxidant Capacity and Total Phenolic Content
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356482/ - Effects of Dietary Fiber and Its Components on Metabolic Health
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257631/ - Whole grain oats, more than just a fiber: Role of unique phytochemicals
https://pubmed.ncbi.nlm.nih.gov/28067025/ - Epidemiology, Etiology, and Treatment of Gastroparesis: Real-World Evidence From a Large US National Claims Database
https://www.sciencedirect.com/science/article/pii/S0016508521036131
- Gastric Stasis
- Gastric Stasis
https://pubmed.ncbi.nlm.nih.gov/29489278//a> - Worldwide prevalence and burden of gastroparesis‐like symptoms as defined by the United European Gastroenterology (UEG) and European Society for Neurogastroenterology and Motility (ESNM) consensus on gastroparesis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9557951/ - Diabetic gastroenteropathy: An underdiagnosed complication
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8192258/ - Malignancy-associated gastroparesis: an important and overlooked cause of chronic nausea and vomiting
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3926490 - Epidemiology, Etiology, and Treatment of Gastroparesis: Real-World Evidence From a Large US National Claims Database
https://www.gastrojournal.org/article/S0016-5085(21)03613-1/fulltext - Foods Provoking and Alleviating Symptoms in Gastroparesis: Patient Experiences
https://link.springer.com/article/10.1007/s10620-015-3651-7 - Diet and Nutrients in Gastrointestinal Chronic Diseases
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7551310/ - Dietary Intake and Nutritional Deficiencies in Patients With Diabetic or Idiopathic Gastroparesis
https://www.gastrojournal.org/article/S0016-5085(11)00600-7/fulltext - Diabetic Gastroparesis: A Review
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428659/ - The Role of Gluten in Gastrointestinal Disorders: A Review
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10096482/ - Analysis of Popcorn (Zea Mays L. var. Everta) for Antioxidant Capacity and Total Phenolic Content
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356482/ - Effects of Dietary Fiber and Its Components on Metabolic Health
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257631/ - Whole grain oats, more than just a fiber: Role of unique phytochemicals
https://pubmed.ncbi.nlm.nih.gov/28067025/ - Epidemiology, Etiology, and Treatment of Gastroparesis: Real-World Evidence From a Large US National Claims Database
https://www.sciencedirect.com/science/article/pii/S0016508521036131
Read full bio of Mary Sabat
Read full bio of Payal Karnik
Read full bio of Ravi Teja Tadimalla
Read full bio of Aparna Mallampalli
























Community Experiences
Join the conversation and become a part of our empowering community! Share your stories, experiences, and insights to connect with other beauty, lifestyle, and health enthusiasts.